MIPS: Simplifying The Merit-Based Incentive Payment System
The Merit-Based Incentive Payment System (MIPS) is the future value-based program for Medicare Part B Providers that should be considered the default Medicare payment program beginning January 1, 2019 with a two-year look-back, therefore truly beginning in 2017. This program rolls up Meaningful Use (MU), the physician quality reporting system (PQRS), and the value-based payment modifier (VBM) into a single program while adding resource-use metrics and Clinical Practice Improvement activity adjustments.
Fee-For-Service Basics
Currently, physicians are reimbursed on a fee-for-service basis, meaning they are paid for each office visit, procedure, or diagnostic test they perform. To maintain financial sustainability in a time of declining reimbursement, physicians are externally influenced to see more patients, perform procedures with higher reimbursement rates even if lower-cost treatment options are equally as effective.
MIPS Basics
CMS will attempt to control Medicare spending by providing pro-active thresholds at the beginning of a reporting period to guide “Eligible Providers” to understand their intended targets. These targets will result in a composite score in 2019 (These weighted categories will be adjusted in the following years):
30 points – Quality (PQRS)-Improvement-Incentives Included
30 points – Resource Use (VBM)
25 points – EHR Meaningful Use (MU)
15 points – Clinical Practice Improvement Activities
In the 2017-2018 performance years, the following Medicare Part B providers are considered eligible professionals:
• Physicians
• Physician Assistants
• Nurse Practitioners
• Clinical Nurse Specialists
• Nurse Anesthetists
2019 and beyond, the following Medicare Part B providers will become eligible professionals:
• Physical & Occupational Therapists
• Speech-language pathologists
• Audiologists
• Nurse Midwives
• Clinical Social Workers
• Clinical Psychologists
• Dietitians and Nutrition Professionals
Exempted providers include:
• 1st year Medicare providers
• Participants in Alternative Payment Models (APMs)
• Providers not meeting the “low volume threshold” (Yet to be Defined-Estimated to be proposed in July 2016)
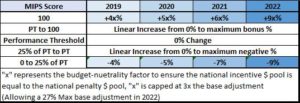
MIPS Reimbursement Impact
Until now, PQRS, MU, and the VBM penalties were largely considered tolerable by many physicians as the initial capital necessary to pursue uncertain rewards largely deterred many providers from participating. Similarly, the vast range of providers falling into “neutral tiers” of these programs allowed physicians to largely ignore their effects; however, the MIPS program is completely budget-neutral, only providers earning the exact threshold score to receive no payment adjustment. Thus, almost every eligible provider will either experience a positive or negative adjustment as the penalized providers will fund the positive adjustments for the providers exceeding the composite threshold.
The 2019 payment-year reflects the 2017 performance year of MIPS. 2018 payment-year will continue to reflect the 2016 performance-year through the separate MU, VBM, and PQRS programs.
The “x” multiplier represents a budget-neutrality factor which provides a bonus-incentive for the highest performing MIPS-providers to earn up to 3x the maximum bonus % each year (Up to 12% in 2019). Keep in mind, CMS contains Medicare costs through the funding the of MIPS “winners” positive adjustments with the “losers” negative adjustments. Furthermore, MIPS scores will be publicly reported on Medicare’s Physician Compare site providing yet another elusive effect considering how these scores may effect patients’ choice of providers in the not-so-distant future.
How do I start preparing for the MIPS program?
85% of the MIPS score reflects the performance measuring mechanisms of MU, PQRS, and VBM. Continuing to focus on these programs by organizing administrative efforts to improve efficiency will assist in your ability to report most successfully. CMS also released the first set of Core Quality Measures signaling a much-needed unification of quality reporting mechanisms amongst payers, we recommend you follow this similar trend closely. If you’re not proactively planning, it is only a matter of time before your reimbursement penalties become someone else’s bonus checks. Stay tuned for further updates.